Chicago Congenital Heart Defect Attorneys
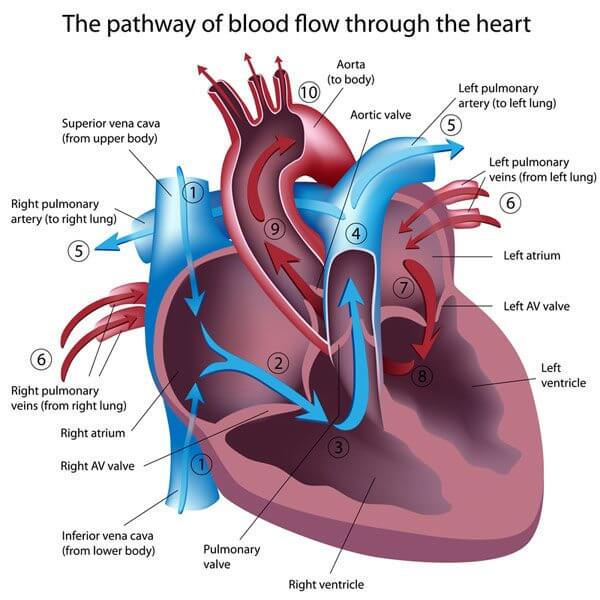
 Of all birth defects, Congenital Heart Defects (CHD) are the most common. All such heart defects can in varying degrees affect the flow of blood through the heart as well as throughout the entire body. These heart defects may vary in severity from a mild CHD, such a tiny hole within the heart, to what is referred to as Critical Congenital Heart Disease (or Critical CHD).
Of all birth defects, Congenital Heart Defects (CHD) are the most common. All such heart defects can in varying degrees affect the flow of blood through the heart as well as throughout the entire body. These heart defects may vary in severity from a mild CHD, such a tiny hole within the heart, to what is referred to as Critical Congenital Heart Disease (or Critical CHD).
Although causes of Congenital Heart Defects are mostly unknown, genetic and chromosomal changes, environmental effects, the mother's health, diet, and pre-existing medical conditions such as obesity, diabetes, and smoking may each play some part.
Millions of adults and children live with CHDs in the United States. Many experience little to no problems with everyday life as a result. Others, especially those with Critical CHDs may require immediate corrective surgery in their first year of life or later in life.
In addition, other medical problems such as an increased risk for heart muscle infection (infective endocarditis), heart weakness (cardiomyopathy), or heart beat irregularity (arrhythmias) may develop over time.
Conditions Caused by Congenital Heart Defects
- Bradycardia occurs when the heart beats slower than normal.
- Tachycardia occurs when the heart beats quicker than normal.
For some patients, prescription medications can greatly improve this condition. For less fortunate patients, invasive heart surgeries will be needed.
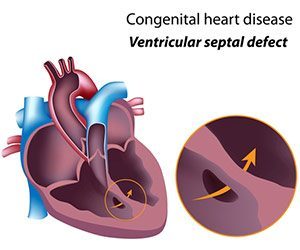 A VSD is a congenital birth defect that appears as a hole in the wall between the two ventricles of the heart. As a result, oxygen-rich blood enters through the septum hole into the left ventricle, mixing both oxygen-rich and oxygen-poor blood and therefore sending extra, oxygen-rich blood to the lungs. The lungs and heart must then work harder.
A VSD is a congenital birth defect that appears as a hole in the wall between the two ventricles of the heart. As a result, oxygen-rich blood enters through the septum hole into the left ventricle, mixing both oxygen-rich and oxygen-poor blood and therefore sending extra, oxygen-rich blood to the lungs. The lungs and heart must then work harder.
Although some small holes will close over time, generally if this condition is not repaired surgically, complications including high blood pressure (pulmonary hypertension), heart failure, stroke, or an irregular heart beat (arrhythmia) may result.
A Ventricular Septal Defect is often diagnosed shortly after birth, although in some cases not until much later in life. In addition to diagnostic tests such as an ultrasound or echocardiogram, some of the signs and symptoms of a VSD may include:
- A whooshing sound called a heart murmur
- Sweating
- Poor weight gain
- Shortness of breath
- Tiredness during feeding
A baby with this birth defect may have a hole in more than one location on the septum. Some of the common names and locations include:
- Muscular Ventricular Septal Defect: The most common type; it involves a hole at the muscular, lower part of the septum.
- Perimembranous Ventricular Septal Defect: A hole located at the upper section of the septum.
- Conoventricular Ventricular Septal Defect: A hole near where the septum should meet the aortic and pulmonary valves.
- Inlet Ventricular Septal Defect: A hole located near where blood will enter the ventricles via the mitral and tricuspid valves.
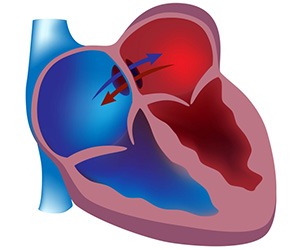 A congenital birth defect that involves a hole in the septum (wall) which divides the upper chambers (atria) of the heart is referred to as an Atrial Septal Defect. This defect may be discovered during pregnancy in an ultrasound, after birth, or in some cases much later in life with an electrocardiogram (EKG). During development, the fetus has many such holes in the heart, but they are supposed to close over time. When they do not close normally, this congenital defect is the result.
A congenital birth defect that involves a hole in the septum (wall) which divides the upper chambers (atria) of the heart is referred to as an Atrial Septal Defect. This defect may be discovered during pregnancy in an ultrasound, after birth, or in some cases much later in life with an electrocardiogram (EKG). During development, the fetus has many such holes in the heart, but they are supposed to close over time. When they do not close normally, this congenital defect is the result.
The Atrial Septal Defect may be very small and virtually unnoticed, requiring no treatment or just medication to treat minor symptoms. In other cases, the hole may be large and require immediate surgery to avoid damage to the blood vessels of the lungs. In rare cases, the hole may be so large and allow so much blood to flow through that it can cause growth issues, excessive fatigue, shortness of breath, or congestive heart failure.
Symptoms and Signs of Atrial Septal Defect
Although many babies are not diagnosed at birth with an Atrial Septal Defect, this untreated condition may result in some of the following signs and symptoms:
- Swelling of feet, legs, or stomach
- Breathing difficulties
- Stroke
- Fatigue while baby is feeding
- Whooshing sound heard by stethoscope
- Missing heartbeats
Treatment for Atrial Septal Defect
Although some smaller holes are treated with medication, larger holes may require open heart surgery, closure by way of a transcatheter device during cardiac catheterization, or FDA approved devices such as the Helex Septal Occluder or the Amplatzer Septal Occluder.
 A congenital birth defect, Truncus Arteriosus is a rare condition that results in one large blood vessel (truncal valve) leading from the heart, rather than two separate blood vessels (pulmonary valve and aortic valve). So, rather than separating completely during the development of the fetus, the blood vessel maintains a connection between the pulmonary artery and the aorta. Babies with this condition also generally have a ventricular septal defect that allows oxygen-rich and oxygen-poor blood to mix together, resulting in excessive blood being pumped to the lungs and the heart working harder to supply blood to the rest of the body.
A congenital birth defect, Truncus Arteriosus is a rare condition that results in one large blood vessel (truncal valve) leading from the heart, rather than two separate blood vessels (pulmonary valve and aortic valve). So, rather than separating completely during the development of the fetus, the blood vessel maintains a connection between the pulmonary artery and the aorta. Babies with this condition also generally have a ventricular septal defect that allows oxygen-rich and oxygen-poor blood to mix together, resulting in excessive blood being pumped to the lungs and the heart working harder to supply blood to the rest of the body.
Symptoms and Signs of Truncus Arteriosus
If left untreated, this condition may be fatal. But surgery is usually successful. During the first few days of life, certain signs and symptoms are generally present which should alert medical personnel of this birth defect. These signs include:
- Excessive sleepiness
- Poor feeding habits
- Cyanosis (blue tint to skin)
- Irritability
- Tachypnea (rapid breathing)
- Pounding heart beat
- Dyspnea (shortness of breath)
Possible Causes of Truncus Arteriosus
Although an exact cause for a congenital birth defect is always difficult to determine, certain factors affecting the pregnant mother are known to increase the risk, including:
- Smoking
- Poorly-managed diabetes
- Contracting a viral illness, such as German measles (rubella)
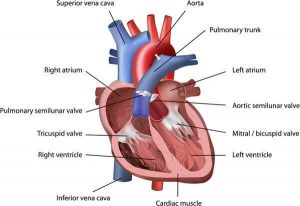
 An Atrioventricular Septal Defect (AVSD) (also known as Atrioventricular Canal Defect, AV Canal Defect, or Endocardial Cushion Defect) is a congenital birth defect which manifests in holes between the left and right heart chambers with abnormalities of the valves controlling the blood flow between those chambers. As a result, lower oxygen blood levels occur, with abnormal amounts of potentially harmful blood flowing to the lungs. This additional blood flow can result in congestive heart failure due to the extra work the lungs and heart must perform.
An Atrioventricular Septal Defect (AVSD) (also known as Atrioventricular Canal Defect, AV Canal Defect, or Endocardial Cushion Defect) is a congenital birth defect which manifests in holes between the left and right heart chambers with abnormalities of the valves controlling the blood flow between those chambers. As a result, lower oxygen blood levels occur, with abnormal amounts of potentially harmful blood flowing to the lungs. This additional blood flow can result in congestive heart failure due to the extra work the lungs and heart must perform.
A high incidence of AVSD occurs in babies with Down syndrome, so diagnostic tests such as an echocardiogram are advised to confirm whether such a congenital defect exists. Depending on which heart structures have abnormally formed, there are two general AVSD types that may occur:
- Incomplete or Partial AVSD involves a hole in the ventricular wall near the heart’s center or a hole in the atrial wall. Although a partial AVSD typically has both tricuspid and mitral valves, one of the valves may not completely close, allowing a backwards leakage of blood from ventricle to atrium.
- Complete AVSD happens when a large central hole in the heart allows blood to flow in between each of the four heart chambers. This hole is located where the walls (septa) that separate the atria (two top chambers) and the ventricles (two bottom chambers) join one another. Instead of two center valves, there is a single center valve instead with flaps (leaflets) that do not close correctly.
Atrioventricular Septal Defects may not be noticed at birth or for years afterwards. Signs that such a condition exists and may be worsening include:
- Pulmonary Hypertension (type of blood pressure condition)
- Arrhythmia (abnormal heart rhythm)
- Congestive Heart Failure (failure of the heart to pump enough oxygen and blood)
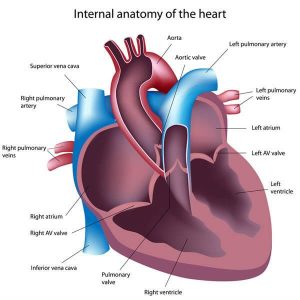
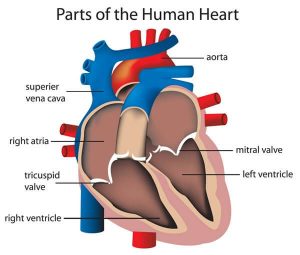 The tricuspid valve is the portion of the heart that controls the flow of blood from the upper right chamber (atrium) to the lower right chamber (ventricle). Tricuspid atresia is a congenital birth defect which results in a valve that does not form at all - instead, solid tissue blocks the opening, so the blood is unable to travel from the right atrium to the corresponding right ventricle, and on to the lungs to retrieve oxygen. This leaves blood needing to find another path to get around the abnormally formed tricuspid valve. Accordingly, most babies born with tricuspid atresia also have a hole known as an atrial septal defect that allows this flow of blood.
The tricuspid valve is the portion of the heart that controls the flow of blood from the upper right chamber (atrium) to the lower right chamber (ventricle). Tricuspid atresia is a congenital birth defect which results in a valve that does not form at all - instead, solid tissue blocks the opening, so the blood is unable to travel from the right atrium to the corresponding right ventricle, and on to the lungs to retrieve oxygen. This leaves blood needing to find another path to get around the abnormally formed tricuspid valve. Accordingly, most babies born with tricuspid atresia also have a hole known as an atrial septal defect that allows this flow of blood.
This congenital defect is considered a critical defect that, depending on the presence of other birth defects and their severity, often requires immediate surgery. Although the following surgeries will not completely cure the condition, they can restore more normal heart functionality:
- Banding: If other heart defects are also present, sometimes there is not enough blood going to the body and too much going to the lungs. This procedure involves a band being placed around an artery to limit the volume going to the lungs.
- Septostomy: Performed early in life, this surgery enlarges or creates an atrial septal defect to allow more blood rich with oxygen to mix with oxygen-poor blood.
- Shunt Procedure: This surgery creates a bypass (known as a shunt) from the aorta to the pulmonary artery to increase blood flow to the lungs.
- Fontan Procedure: Usually performed around age two, this surgery connects the inferior vena cava and the main pulmonary artery to the heart.
- Bidirectional Glenn Procedure: This surgery connects the superior vena cava and the main pulmonary artery to the heart.
 Coarctation refers to a narrowing of the aorta, which is the major artery leading from the heart. As this artery is responsible for pumping blood from the heart to vessels throughout the body, any such restriction in the passage can result in serious medical issues.
Coarctation refers to a narrowing of the aorta, which is the major artery leading from the heart. As this artery is responsible for pumping blood from the heart to vessels throughout the body, any such restriction in the passage can result in serious medical issues.
This congenital birth defect is more common in people with genetic disorders like Turner syndrome and affects about four out of every 10,000 babies born each year. It is often related to cerebral aneurysms as well as other heart defects.
- Ventricular Septal Defect
- Defects where there is only a single ventricle
- Bicuspid Aortic Valve
Diagnostic Tests
Although a coarctation of the aorta may be discovered soon after birth, it is usually not discovered until the child is much older. Some of the medical tests used to diagnose this congenital condition include:
- Blood pressure testing to determine if the pressure in the arms is stronger than that in the legs
- Checking if femoral (groin) pulse is weaker than carotid (neck) pulse
- Chest x-rays
- Aortography and cardiac catheterization
- Echocardiography
- MR Angiography (MRI)
- Heart CT
Possible Complications
This condition is considered a critical Congenital Heart Defect (CHD) and often requires surgery. A number of surgical options are available, including balloon angioplasty and end-to-end anastomosis. But as with any serious surgery, complications can arise:
- Endocarditis
- Continued narrowing of the aorta
- Stroke
- High blood pressure
- Kidney problems
- Lower body paralysis
- Aortic aneurysm
- Brain bleeding
- Heart failure
- Aortic rupture
- Aortic dissection
 This is a congenital heart birth defect in which oxygen-rich blood from the lungs does not return to the left atrium, but instead goes into the right side of the heart. This oxygen-rich blood mixes with the oxygen-poor blood. As a result, less oxygen is supplied to the body. This birth defect is called total anomalous pulmonary venous return (TAPVR).
This is a congenital heart birth defect in which oxygen-rich blood from the lungs does not return to the left atrium, but instead goes into the right side of the heart. This oxygen-rich blood mixes with the oxygen-poor blood. As a result, less oxygen is supplied to the body. This birth defect is called total anomalous pulmonary venous return (TAPVR).
Babies with TAPVR many times have an atrial septal defect (hole) that allows this mixed blood to reach the left side of the heart, where it then gets pumped out throughout the body. Depending on where the pulmonary veins connect abnormally to the heart, three different types of total anomalous pulmonary venous return exist. These include:
- Cardiac TAPVR: Pulmonary veins connect to the right atrium and meet behind the heart.
- Supracardiac TAPVR: Pulmonary veins form an abnormal connection and meet above the heart at the superior vena cava.
- Infracardiac TAPVR: Pulmonary veins form an abnormal connection and meet below the heart.
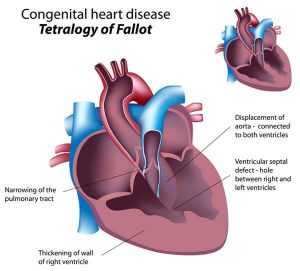 "Tetra" means four. In this critical congenital birth defect, four heart defects combine to reduce the proper flow of oxygen-rich blood to the body. The four congenital defects are:
"Tetra" means four. In this critical congenital birth defect, four heart defects combine to reduce the proper flow of oxygen-rich blood to the body. The four congenital defects are:
- Pulmonary Stenosis: A narrowing of the main pulmonary artery and pulmonary valve;
- Ventricular Septal Defect: A hole in the wall that separates ventricles (two lower chambers) of the heart;
- Ventricular Hypertrophy: A thickening of the muscular wall of the right ventricle;
- Enlarged aortic valve which appears to open from both ventricles rather than from only the left ventricle.
Because of the severity of this defect, surgery is usually performed soon after birth. This surgery may include a replacement or widening of the pulmonary valve along with an enlargement of the accompanying pulmonary artery. A patch over the ventricular septal defect will further improve blood flow.
Some babies with Tetralogy of Fallot may have:
- Cyanosis: bluish skin
- Tet spells: suddenly develop bluish skin when agitated or after feeding
- Delayed development and growth
- Fainting, seizures, or dizziness
- Arrhythmia: irregular heart beat
- Endocarditis: higher risk for heart infection
 A critical congenital heart defect that occurs in only about 1 of every 3,000 U.S. born babies each year, d-TGA is an abnormality involving the two main arteries carrying blood from the heart. In this defect, the aorta and the main pulmonary artery are transposed, or switched, and connected to the wrong heart chambers.
A critical congenital heart defect that occurs in only about 1 of every 3,000 U.S. born babies each year, d-TGA is an abnormality involving the two main arteries carrying blood from the heart. In this defect, the aorta and the main pulmonary artery are transposed, or switched, and connected to the wrong heart chambers.
Normally, blood is carried throughout the body in this cycle: body -> heart -> lungs -> heart -> body. In the case of d-TGA, the cycle is either:
- Body -> heart -> body: This results in a cycle without blood being sent to the lungs for oxygen;
- Lungs -> heart -> lungs: This results in a cycle without oxygen being properly delivered throughout the body.
Symptoms & Treatment of dextro-Transposition of the Great Arteries
This birth defect is usually apparent at birth or very soon after and almost always requires prompt surgery to remedy. Commonly, it is diagnosed with an echocardiogram or newborn pulse oximetry screening. But, even before such diagnostic testing is performed, physical symptoms often reveal the existence of this birth defect, such as:
- Breathing problems
- Weakened pulse
- Bluish or ashen skin coloring (cyanosis)
- Heart palpitations
- Inability to feed properly
Types of Pulmonary Atresia
There are two typical types of pulmonary atresia depending on whether the baby has a hole in the wall of the heart ventricles. They are:
- Pulmonary atresia with intact ventricular septum: In this type, the septum (or wall) between the ventricles is intact and complete with a right ventricle that is very small and remains underdeveloped.
- Pulmonary atresia with VSD: In this type, a ventricular septal defect allows the flow of blood in and out of the right ventricle during pregnancy, so the pulmonary artery is not as small as atresia with an intact septum.
- Very small or unformed mitral valves
- Undersized or underdeveloped left ventricle
- Very small or unformed aortic valve
- Undersized or underdeveloped ascending portion of aorta
- Babies with HLHS will often also have an atrial septal defect as well
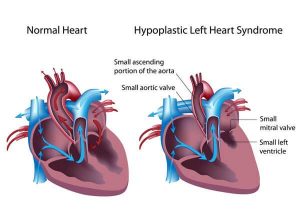 In order to bypass the poorly-functioning left heart and increase blood flow throughout the body, a series of surgeries are usually undertaken, including:
In order to bypass the poorly-functioning left heart and increase blood flow throughout the body, a series of surgeries are usually undertaken, including:
- The Norwood Procedure: Usually performed during the first two weeks of life, the surgeon creates and connects a new aorta to the right ventricle, as well as a tube to the pulmonary arteries.
- The Bidirectional Glenn Shunt Procedure: Usually performed between four and six months of age, the surgeon directly connects the pulmonary artery and the superior vena cava.
- The Fontan Procedure: Usually performed between eighteen months and three years old, the surgeon connects the pulmonary artery and inferior vena cava to the heart.
Did a Physician Misdiagnose Your Child's Congenital Heart Defect?
In order to prevent the devastating effects of congenital heart defects, the most prominent medical associations recommend an echocardiogram. A pediatric cardiologist should perform this relatively simple procedure that can identify signs of heart defects before a child's birth. Frequently, these severe heart defects are diagnosed as heart murmurs by mistake, preventing the child from receiving immediate care from a trained cardiologist. If a physician fails to order an echocardiogram and a child is born with a congenital heart defect, the doctor in charge may be held liable for medical malpractice.
In order to improve a child's chances of survival, heart surgery will usually be required to address the defect. If surgery is performed too late due to a physician's failure to order an echocardiogram, the afflicted newborn's chances of survival will plummet. Even if the child does survive, he or she could be facing a variety of severe medical conditions for the rest of their lives. These medical conditions can be life-threatening, expensive, painful, and emotionally damaging.
Certain congenital heart defects, in particular, ventricular septal defects, require immediate medical attention. Many of these defects can lead to severely damaging and potentially lethal medical conditions, such as pulmonary hypertension. Research even shows that even if a child does survive their infant years with such a condition, he or she will have a significantly lower life expectancy than healthy peers.
What Should You Do if Your Child Suffers From a Congenital Heart Defect?
If your son or daughter was accidentally diagnosed with a heart murmur, but in reality, they were suffering from a congenital heart defect, you may have a case. If you believe that your child's heart defect was diagnosed too late, contact the Chicago birth defect lawyers at Sexner Injury Lawyers LLC at (312) 243-9922.